Hemorrhoid Care
What are hemorrhoids?
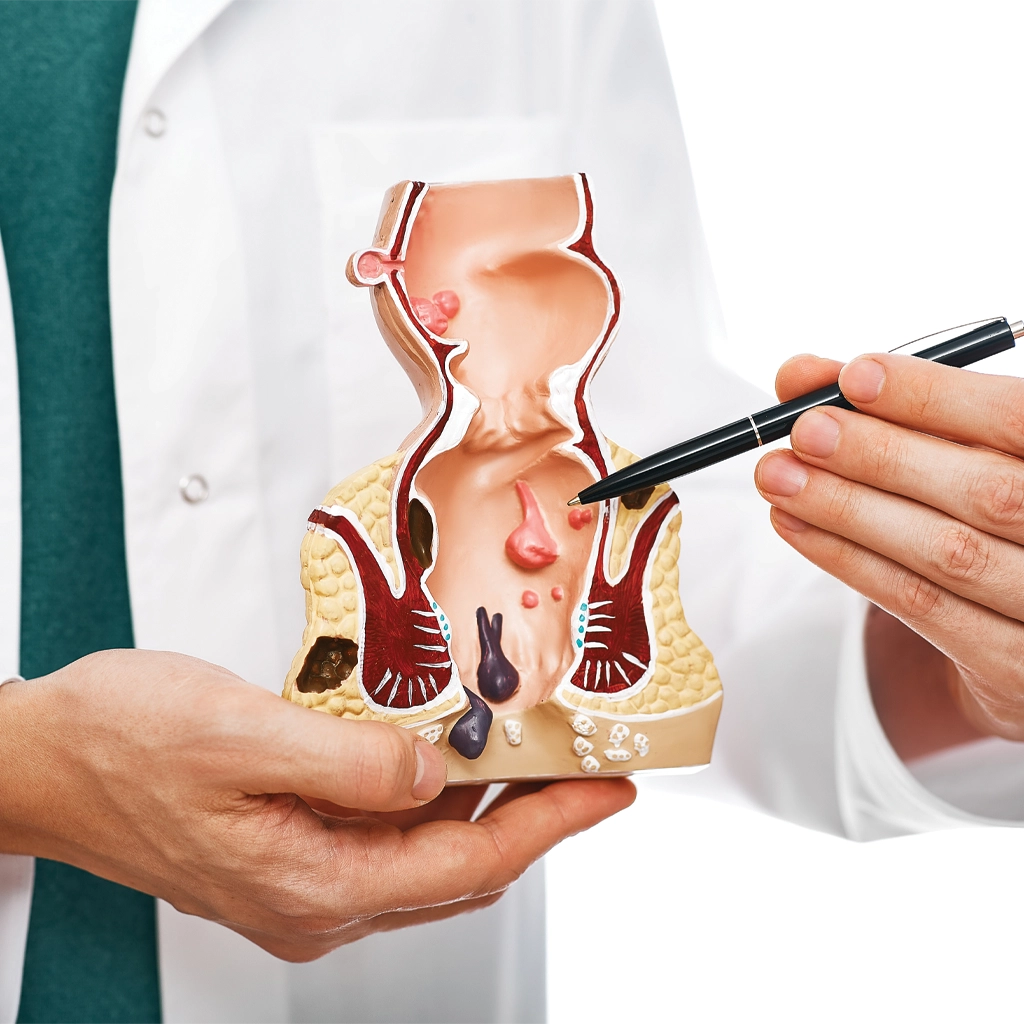
Hemorrhoids are swollen veins in the anus and lower rectum. As they grow, they can be painful and itchy, and interfere with bowel movements. They can also bleed. National Vascular Physicians invites you to learn more about hemorrhoid care with the resources on this page.
Do hemorrhoids go away on their own?
Most hemorrhoids will go away on their own, but for some, they persist for weeks and do not respond to topical treatments like hemorrhoid care creams and sitz baths. These are called chronic hemorrhoids.
What is Hemorrhoidal Artery Embolization (HAE)?
HAE is a minimally invasive procedure used to treat chronic hemorrhoids, a condition characterized by swollen and inflamed blood vessels in the rectal area. HAE is primarily performed as an alternative to traditional surgical interventions such as hemorrhoidectomy.
Read more about our non-surgical solution for hemorrhoid care »

What causes hemorrhoids?
Most people have the wrong idea about hemorrhoids. Hemorrhoids are actually swollen veins inside the lower rectum or under the skin around the anus, similar in nature to varicose veins. They most commonly occur in those between 45 and 65 years of age. They may be caused by an increase in pressure in the lower rectum through one or more of the following factors:
- Sitting for long periods
- Straining or excessive exercise
- Spinal cord injury
- Constipation or diarrhea
- Being overweight
- Pregnancy or childbirth
- Family history
A diet high in fiber, as well as drinking plenty of fluids and getting regular exercise can help prevent hemorrhoids.
Common Symptoms Associated with Hemorrhoids
- None – many people with hemorrhoids have no symptoms.
- Itching of the skin around the anus
- Bright red blood after using the toilet which is often painless
- Pain if a blood clot forms inside a hemorrhoid. In this case, you may also feel a lump
- Swelling of hemorrhoids outside of the rectum (prolapse) during a bowel movement
Who suffers from hemorrhoids?
About half of all Americans will experience hemorrhoids in their lifetimes. In most cases, hemorrhoids will go away on their own or with diet changes, topical treatments, medications or supplements. But they can also persist and cause bleeding, itching and painful bowel movements.
If conservative hemorrhoid care treatments have failed and symptoms persist, the potential complications of hemorrhoids and resulting painful conditions can include:
- Perianal thrombosis
- Incarcerated prolapsed hemorrhoids
- Anemia
- Blood clots
- Blood loss (due to a burst hemorrhoid)
- Infection
- Skin tags
What are my hemorrhoid treatment options?
Conservative treatment for hemorrhoids may include diet changes, topic treatments (such as an over-the-counter hemorrhoid cream), sitz baths and oral pain relievers (such as Tylenol). If the symptoms do not disappear, and if you are experiencing severe pain, bleeding, changes in bowel habits or changes to the color or consistency of your stools, you will want to talk with your doctor about other treatment options.
When conservative treatment has failed, hemorrhoidectomy is a surgical procedure to remove them. However, surgery comes with risks and complications that can include infection, bleeding, difficulty emptying the bladder, rectal prolapse and more.1.2 Recovery takes at least 2 weeks, and it can be as long as 3-6 weeks before you feel normal again.
Another procedure, called rubber band ligation, is a less invasive technique that has been used more commonly in the last few years. However, this approach is also associated with pain and complications, especially for those taking anti-platelet or anti-coagulant medication and who have a higher risk of hemorrhage and infectious complications.3
A new and minimally invasive option to treat hemorrhoids is called Hemorrhoidal Artery Embolization (HAE). This is typically recommended for patients with grade 1 to 3 internal hemorrhoids who have not responded to conservative hemorrhoid care.

- Hiroko Kunitake, MD, MPH and Vitaliy Poylin, MD, FACS, FASCRS2 Complications Following Anorectal Surgery Clin Colon Rectal Surg. 2016, Mar; 29(1): 14-21.
- Christos Simoglou et al. Milligan-Morgan Haemorrhoidectomy Complications. Hellenic Journal of Surgery 86, 68-71
- Andreia Albuquerque Rubber band ligation of hemorrhoids: A guide for complications. World J Gastrointest Surg. 2016 Sep 27; 8(9): 614-620
- Sandeep Bagla, MD et al. Outcomes of Hemorrhoidal Artery Embolization from a Multidisciplinary Outpatient Interventional Center. Journal of Vascular and Interventional Radiology. February 1, 2023.
Hemorrhoidal Artery Embolization
Hemorrhoidal Artery Embolization (HAE) is a minimally invasive procedure used to treat hemorrhoids. Hemorrhoids are swollen veins in the rectum and anus that can cause discomfort, bleeding, and pain.
During the HAE procedure, an interventional radiologist inserts a small catheter into the artery from the groin or wrist and navigates it to the superior rectal artery, which supplies blood to the hemorrhoids. Once the catheter is in place, the radiologist places small metallic coils or medical beads into the artery to block blood flow to the hemorrhoids.
Without blood flow, the hemorrhoids shrink and eventually disappear. HAE is a safe and effective treatment option for hemorrhoids, with high success rates and minimal complications. Patients typically experience little to no pain after the procedure and can return to their normal activities within a few days.
HAE is an attractive option for patients who have failed to find relief with traditional treatments, such as creams, ointments, and suppositories, or who do not want to undergo surgery.
The Hemorrhoidal Artery Embolization (HAE) procedure
HAE is performed by an interventional radiologist who inserts a tiny catheter into an artery in your upper thigh and then uses x-ray imaging to guide it through the body’s blood vessels to the rectal artery. Special coils are inserted into the artery to cut off the blood supply to the hemorrhoid, causing it to shrink. The success rate of this procedure is greater than 90%.4
Unlike surgery, there is no general anesthesia required for the procedure, no incisions and no scarring. You are able to return home the same day and resume your normal activities.
Talk to your doctor about HAE for hemorrhoid care
This procedure is performed on an outpatient basis by the experienced doctors at National Vascular Physicians. If your doctor is not familiar with Hemorrhoidal Artery Embolization, we are happy to help provide them with the information they need to make an informed recommendation.
Our doctors are fellowship trained in vascular and interventional radiology. With more than 13 years of education and training, they are among the most highly trained doctors practicing medicine today and are uniquely qualified to provide both diagnostic evaluations as well as the required treatment.
If you believe you are a candidate for HAE, we invite you to schedule a consultation with us. We are happy to work with your doctor(s) and other members of your care team to find the right treatment for your specific condition.
For more information about HAE for hemorrhoid care, please call 301-276-5670 or click the button below to schedule an appointment.
Hemorrhoidal Artery Embolization (HAE) has several benefits for the treatment of hemorrhoids, including:
- Minimally invasive: HAE is a minimally invasive procedure, which means it is performed using a small incision and does not require general anesthesia. This results in a shorter hospital stay and a faster recovery time than traditional surgery.
- High success rates: HAE has high success rates in treating hemorrhoids, with studies reporting success rates of up to 90%. This means that most patients experience significant improvement in their symptoms after the procedure.
- Minimal pain and discomfort: HAE is associated with minimal pain and discomfort compared to traditional surgery, and patients typically require only mild pain medication after the procedure.
- Reduced risk of complications: HAE has a lower risk of complications compared to traditional surgery, such as bleeding, infection, and incontinence.
- Suitable for all types of hemorrhoids: HAE can be used to treat all types of hemorrhoids, including internal, external, and mixed hemorrhoids.
- Outpatient procedure: HAE can be performed as an outpatient procedure, meaning that patients can return home the same day as the procedure.
- Quick recovery time: Most patients can return to their normal activities within a few days after the procedure, which is significantly faster than traditional surgery.
What is the research on HAE for hemorrhoid care?
Various studies have demonstrated the effectiveness of HAE in the treatment of hemorrhoids. These studies have shown that HAE can effectively reduce the size of hemorrhoids, relieve symptoms, and improve patients’ quality of life. Other studies have compared HAE with other treatment modalities, such as rubber band ligation or hemorrhoidectomy. These studies suggest that HAE may offer similar effectiveness in reducing symptoms and improving hemorrhoid-related quality of life compared to traditional surgical interventions without the risks and side-effects associated with surgery.
Overall, HAE is a safe and effective treatment option for hemorrhoids that offers several benefits over traditional surgery, including minimal pain and discomfort, reduced risk of complications, and a faster recovery time.
You may be a candidate for HAE if:
- You have pain from hemorrhoids
- You have bleeding from hemorrhoids
- You feel dilated veins in your anus
- Do not want surgery
Hemorrhoidal Artery Embolization (HAE) is a minimally invasive procedure used to treat severe cases of hemorrhoids.
Benefits of Hemorrhoidal Artery Embolization (HAE) for Hemorrhoid Care
- Non-Surgical Approach: HAE is a non-surgical alternative to traditional hemorrhoid treatments like surgery. It involves blocking the blood supply to the hemorrhoidal tissue, leading to its shrinkage and alleviation of symptoms.
- Effective Hemorrhoid Reduction: HAE has shown promising results in reducing the size and symptoms of hemorrhoids. It can provide relief from rectal bleeding, pain, and swelling associated with severe hemorrhoids.
- Minimally Invasive: HAE is a minimally invasive procedure that is performed under local anesthesia. It involves inserting a catheter into the blood vessels supplying the hemorrhoidal tissue and delivering small particles or coils to block the blood flow.
- Shorter Recovery Time: Compared to traditional surgery, HAE typically offers a shorter recovery period. Patients may experience minimal discomfort and can resume their normal activities relatively quickly.
Risks and Considerations of Hemorrhoidal Artery Embolization (HAE) for Hemorrhoid Care
- Infection and Bleeding: As with any medical procedure, there is a risk of infection and bleeding at the site of catheter insertion. However, these complications are relatively rare.
- Allergic Reactions: Some patients may have an allergic reaction to the contrast dye used during the procedure. It is important to inform the healthcare provider about any known allergies beforehand.
- Tissue Necrosis: In rare cases, the blocked blood supply to the hemorrhoidal tissue may lead to tissue necrosis or death. However, proper patient selection and skilled medical professionals minimize this risk.
- Limited Availability: HAE is a specialized procedure that may not be widely available in all healthcare settings. It is important to consult with a vascular expert or specialist experienced in performing HAE.