Uterine Fibroids & Women’s Health
What are uterine fibroids?
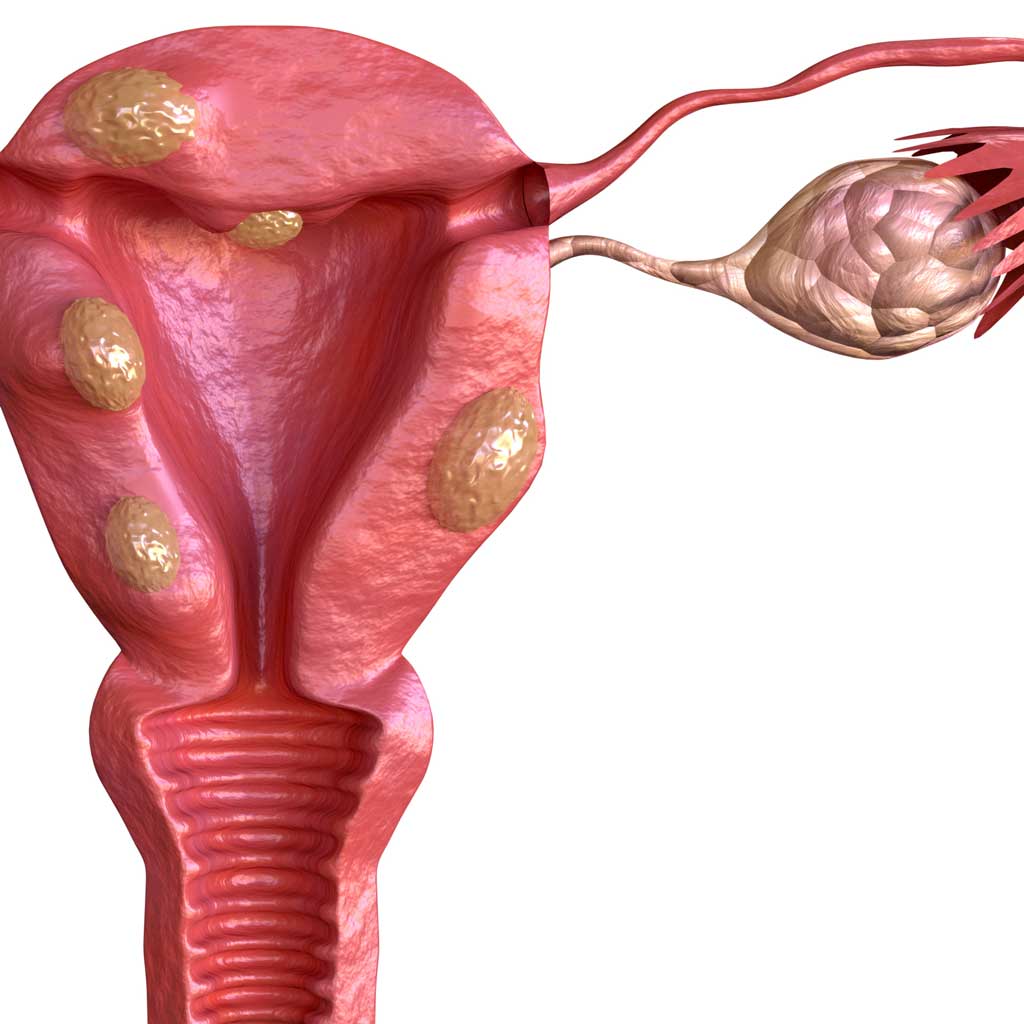
Fibroids, also known as uterine fibroids, leiomyomas, or myomas, are benign (non-cancerous) tumors that grow within the muscle tissue of the uterus.
Who is at risk for uterine fibroids?
Uterine fibroids are the most common tumors within the female reproductive system. 70-80% of women will develop fibroids. Women of African descent are 2-3 times more likely to develop uterine fibroids as women of European descent.
What does the research say about uterine fibroids?
-
Uterine fibroids are the most common diagnosis for women undergoing hysterectomy
-
Success rate of uterine fibroid embolization approaches 90%
-
Uterine fibroid embolization is safely performed in an outpatient basis
-
The American College of Obstetrics and Gynecology (ACOG) recognizes uterine fibroid embolization as a safe and effective treatment for fibroids
Patient Stories: Uterine Fibroids
Judy’s UFE Story
Shantice’s Story
Victoria’s Story
Pam’s UFE Story
Uterine Fibroids Symptoms
Common symptoms of fibroids include:
Heavy Bleeding During Menstrual Cycle
Heavy bleeding during your period is one of the most common symptoms associated with uterine fibroids. Over time, excessive menstrual bleeding may lead to fatigue and anemia, which is a low red blood cell count. If left untreated, heavy bleeding may lead to the need for blood transfusions.
A normal menstrual cycle occurs every 25-31 days and lasts from 3-7 days. Heavy periods are considered when:
- Soaking through one or more sanitary pads or tampons every hour for several consecutive hours
- Bleeding for more than 5 days
- Needing to use double sanitary protection to control menstrual flow
- Needing to wake up to change during the night
- Passing blood clots
- Experiencing signs of anemia like fatigue, brain fog, migraine-like headaches, and chewing/craving ice
Pelvic Pain and Pressure
As fibroids grow, they can put additional pressure on the surrounding organs, which can be extremely painful. The growth of the fibroids can cause consistent lower abdominal pain, as well as swelling which is sometimes mistaken as weight gain or pregnancy.
Urinary Incontinence or Frequent Urination
One of the organs commonly affected during the growth of fibroids is the bladder. As added pressure is applied to the bladder, the risk of urinary incontinence (loss of bladder control) occurs, as well as frequent urination.
Other Symptoms of Uterine Fibroids
Other common symptoms include anemia, pain in the back of the legs, pain during sex, constipation, and an enlarged abdomen.
There are 4 Primary Types of Fibroids
Submucosal
These fibroids develop under the lining of the uterine cavity. Large submucosal fibroid tumors may increase the size of the uterus cavity and can block the fallopian tubes, which can cause complications with fertility. Associated symptoms with submucosal fibroids include very heavy, excessive menstrual bleeding and prolonged menstruation. These symptoms can also cause the passing of clots and frequent soiling accidents. Untreated, prolonged or excessive bleeding can cause more complicated problems such as anemia and/or fatigue, which could potentially lead to a future need for blood transfusions.
Pedunculated
This type of uterine fibroid occurs when a fibroid tumor grows on a stalk, resulting in pedunculated submucosal or subserosal fibroids. These fibroids can grow into the uterus and/or outside of the uterine wall. Symptoms associated with pedunculated fibroid tumors include pain and pressure as the fibroid may sometimes twist on the stalk.
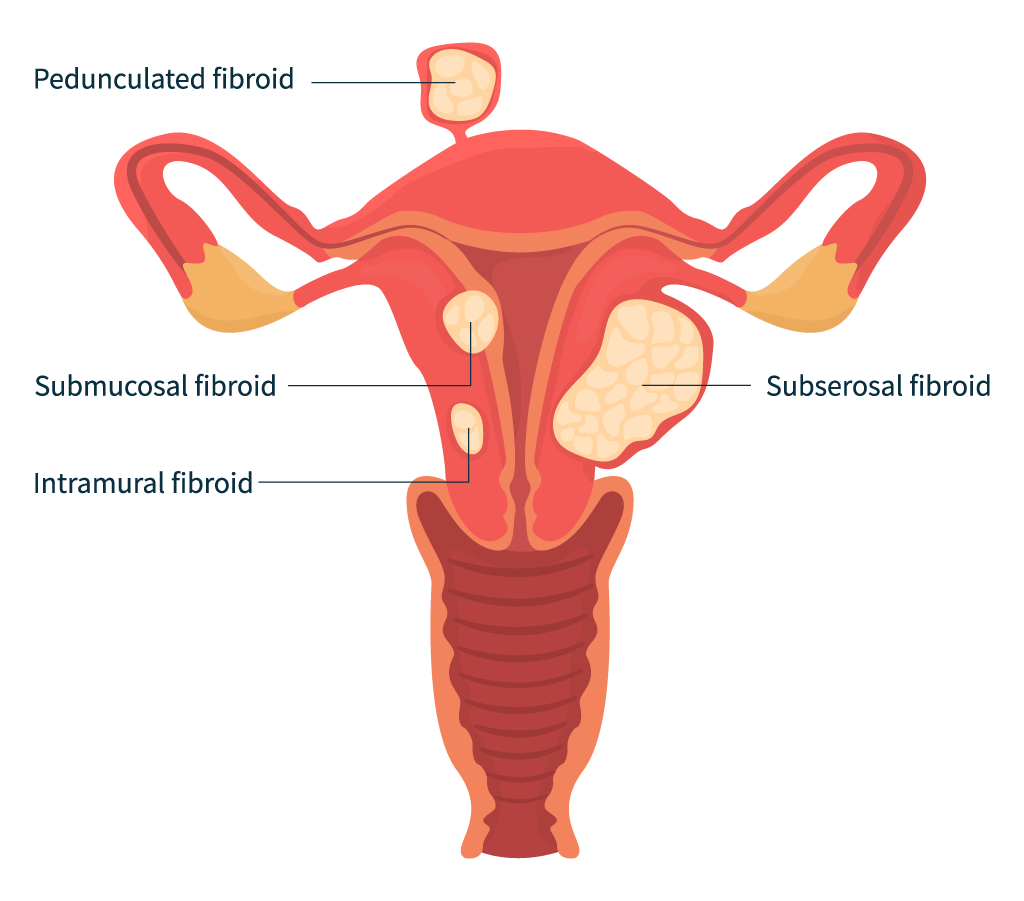
Intramural
The most common type of fibroids, intramural fibroid tumors, typically develop within the uterine wall and expand from there. When an intramural fibroid tumor expands, it tends to make the uterus feel larger than normal, which can sometimes be mistaken for pregnancy or weight gain. This type of fibroid tumor can also cause “bulk symptoms” which include excessive menstrual bleeding that may cause prolonged menstrual cycles and clot passing, and pelvic pain that is caused by the additional pressure placed on surrounding organs by the growth of the fibroid.
Subserosal
Subserosal fibroids typically develop on the outer uterine wall. This type of fibroid tumor can continue to grow outward and increase in size. The growth of a subserosal fibroid tumor will put additional pressure on the surrounding organs, causing pelvic pain and pressure, and tend not to interfere with a women’s typical menstrual flow. Depending on the severity of the location of the fibroids, other complications may accompany pain and pressure such as bloating, indigestion, constipation, and frequent urination.
A woman may have one or all of these types of fibroids. Some fibroid tumors don’t produce any symptoms at all, while others can be severely symptomatic. It is common for a woman to have multiple fibroid tumors and it may be difficult to understand which fibroid is causing specific symptoms.
Treatment of Fibroids: Uterine Fibroid Embolization (UFE)
If you have uterine fibroids, it is a good idea to discuss the various treatment options available for fibroids, including uterine fibroid embolization (UFE).
What is Uterine Fibroid Embolization (UFE)?
The UFE procedure, also known as uterine artery embolization (UAE), begins with a tiny pinhole in the groin or wrist. Using specialized X-ray equipment, an Interventional Radiologist (IR) guides a catheter (small tube) to the uterine arteries. Then, small medical beads are injected through the catheter into the vessels feeding the fibroid, cutting off its blood supply. This shrinks the fibroid(s). The catheter is then removed. The entire UFE treatment typically lasts less than one hour and is an outpatient procedure. Recovery only takes a few days.
Is uterine fibroid embolization (UFE) right for me?
You may be a candidate for UFE if:
- You are experiencing symptoms associated with uterine fibroids
- You want to retain your uterus and are looking for alternatives to hysterectomy
- You do not want surgery
- You are a non-surgical candidate due to a preexisting conditions such as obesity, bleeding disorders, or anemia
- You are not pregnant
Look beyond hysterectomy and discover UFE.
A highly effective, minimally invasive procedure, UFE takes less than an hour to perform. Clinically proven to reduce the major symptoms of uterine fibroids, UFE has become one of the most successful alternatives to hysterectomy procedures.
IS UFE RIGHT FOR YOU? Take our short quiz.
Key Advantages
UFE is a safe treatment option and like other minimally invasive procedures has significant advantages over conventional open surgery. That’s why 90% of all women were “satisfied” or “very satisfied” at final follow-up after UFE.
Benefits of UFE Treatment
- Preservation of the uterus
- Decrease in heavy menstrual bleeding from symptomatic fibroids
- Decrease in urinary dysfunction
- Decrease in pelvic pain and/or pressure
- Virtually no blood loss
- Typically performed as an outpatient procedure
- Offers a shorter hospital stay and a faster return to work when compared to having a hysterectomy
- Safe procedure that involves minimal risk and fewer complications after 30 days when compared to having a hysterectomy
- Overall, significant improvement in patient’s physical and emotional well-being
- Covered by most insurance companies
Risks of UFE
Although UFE complications are rare, any medical procedure carries some degree of risk. Despite the low risk factor, it is important to understand the potential complications associated with UFE. These include:
- Embolization of non-target organs (bowel, bladder, nerves, and buttock)
- Sexual dysfunction related to non-target embolization (cervicovaginal branch)
- Transient amenorrhea (absence of period)
- Common short-term allergic reaction/rash
- Vaginal discharge/infection
- Possible fibroid passage (transcervical passage of fibroid; can cause discharge, cramps, and possible urinary retention)
- Post-embolization syndrome (post-procedure pain, fever, tiredness, and elevated white blood cell count)
- Premature menopause
The effects of UFE on the ability to become pregnant and carry a fetus to term, and on the development of the fetus, have not been determined. As with any medical procedure, discuss all risks and complications with your physician.
Uterine Fibroid Embolization FAQs
Fibroids are benign (non-cancerous) growths that women can develop in and around the uterus. They can be very small or grow to be as large as melon. Fibroids are not life-threatening and may never cause symptoms. But for some, they can cause extreme pain and discomfort and heavy menstruation. They can also prevent a woman from becoming pregnant. When fibroids begin to impact a woman’s quality of life, she may wish to seek treatment.
Many women mistakenly believe that hysterectomy (surgical removal) is the only way to get rid of fibroids and their symptoms. In reality, there are several options for treating fibroids, ranging from medications or surgery to a minimally invasive procedure called uterine fibroid embolization (UFE).
UFE is a non-surgical outpatient procedure that is clinically proven to treat uterine fibroids. It works by cutting off the blood supply to the fibroids, causing them to shrink and symptoms to go away. It does not require uterus removal and is recommended by the American College of Obstetricians and Gynecologists (ACOG).
During the procedure, a doctor known as an interventional radiologist uses imaging to guide the placement of a catheter through the skin in the wrist or upper thigh and into the arteries that carry blood to the fibroid. Microparticles are then injected into these arteries, blocking the flow of blood to the gland. Starved of oxygenated blood, the fibroids shrink, relieving symptoms.
UFE is clinically proven to achieve significant or total symptom relief for about 90% of women who have the procedure. It is effective for women with large or multiple fibroids, and the possibility of fibroids returning is rare.
Pregnancy is possible after UFE; in fact, it can be fertility-restoring for women whose fibroids interfere with their ability to become pregnant. Studies have shown that UFE can improve chances of pregnancy for women with uterine fibroids.
Yes, the procedure is covered by most private insurance and Medicare. If you have any questions related to your specific insurance covering the procedure, please contact us!
UFE is very safe and serious complications are extremely rare. Some women may experience pain or cramping, nausea and/or fever after their procedure. Other rare complications can include injury to the uterus, premature menopause and ovarian failure.
Women who have been diagnosed with fibroids and who have symptoms are eligible for the UFE procedure.
Women with an active pelvic infection, endometrial cancer and chronic kidney disease may not be eligible for UFE. Also, women with fibroids located in certain areas of the uterus may benefit from a different treatment.
Our doctors are among the most experienced in the region, having performed thousands of embolization procedures. We operate two outpatient centers (National Harbor, MD and Roanoke, VA) for your convenience. Our outpatient locations are comfortable and convenient, and we consistently deliver a high level of patient service.
Non Invasive Treatment Options
Watchful Waiting for Asymptomatic Fibroids
If your fibroids do not cause symptoms, there is no need to treat them. Your doctor can best manage your care and can continue to monitor your fibroids for growth.
Hormone Treatment
Medications for fibroids target hormones that regulate a woman’s menstrual cycle and help treat symptoms such as heavy menstrual bleeding and pelvic pressure. They don’t eliminate fibroids, but may shrink them. The possible side effects of using these medications are similar to the symptoms experienced during and after menopause and include: weight gain, hot flashes, vaginal dryness, mood swings, changes in metabolism, and infertility. In most cases, once hormone therapy stops, fibroids tend to grow back and can reach their original size. This often occurs if hormone therapy is not accompanied by another treatment.
High-Intensity Focused Ultrasound Surgery (HIFU or MRgFUS)
During the treatment, magnetic resonance images are used to help a doctor examine fibroids and surrounding organs in 3-D. High-intensity focused ultrasound waves are then used to heat an area of the fibroid, causing cell death. Pulses of ultrasound energy are also applied repeatedly to treat the fibroid. The procedure takes three to four hours. Patients report abdominal pain, cramping, and nausea throughout the procedure. A few days after the procedure, patients report feeling cramps as well as shoulder and back pain. Most women are able to return to work within one to two days following the surgery.
Minimally Invasive Fibroid Treatment Options
Endometrial Ablation
This procedure destroys the endometrium (the lining of the uterus) with the goal of reducing menstrual flow. In some women, menstrual flow may completely stop. No incisions are needed for endometrial ablation, as a physician inserts a slender tool through the cervix. The tools used for this procedure vary depending on the method used. Some types of endometrial ablation use extreme cold, while others depend on heated fluids, microwave energy, or high-energy radio frequencies. This procedure can only be used to treat submucosal fibroids that are less than one inch in diameter.
Surgical Myomectomy Treatments
A myomectomy is the surgical removal of fibroids in the uterus. This treatment is recommended for women who want to become pregnant. There are different types of myomectomy procedures, including:
Hysteroscopic Myomectomy
In this procedure a long, thin scope with a camera and light is passed through the vagina and cervix into the uterus. No incision is needed. Submucosal or intracavitary fibroids can be resected or removed using a wire loop or similar device. Patients are usually sent home following the procedure. The hospital stay is generally under two hours, and recovery time is one or two days. Usually only small fibroids accessible through the cavity can be treated this way.

Laparoscopic Myomectomy
The laparoscope is a slender telescope inserted through the navel (belly button) to view the pelvic and abdominal organs. Two or three half-inch incisions are made below the pubic hairline and instruments are passed through these incisions to perform the surgery. Next, a small scissors-like instrument is used to open the thin covering of the uterus, where the fibroid is found and removed. After the fibroid is removed from the uterus, it is brought out of the abdominal cavity. This is done by cutting the fibroid into small pieces. The pieces are then removed through one of the incisions. Most women are able to leave the hospital the same day as surgery. For more extensive surgery, a one-day stay may be required. Patients can usually walk on the day of surgery, drive in about a week, and return to normal activity within two weeks.
Robotic-assisted Myomectomy
During this procedure, a surgeon sits at a special console with hand and foot controls that move robotic arms during the operation. With the assistance of the robot, the surgeon injects medication into the fibroids to decrease overall bleeding and makes an incision in the uterus. The surgeon then removes the fibroid(s) from the surrounding uterine tissue. Once the fibroid has been removed, the surgeon cuts the fibroid into smaller pieces inside the abdomen, and removes the fibroid pieces through the incision. Patients typically go home the same day of the procedure and most patients resume normal activities within two weeks.
Abdominal Myomectomy
The operation begins with a surgeon entering the pelvic cavity through one or two incisions. Depending on the size and location of the fibroid, a vertical or horizontal incision is made. For large fibroids or fibroids that are located in a ligament between the uterus and pelvic wall, a vertical incision is required. The incision is made from the middle of the abdomen that extends below the navel (belly button). In other cases, a horizontal bikini-line incision is made that runs about an inch above the pubic bone. The procedure usually requires a hospital stay of two to three days. Recovery takes four to six weeks.
Surgical Hysterectomy Treatments
A hysterectomy is a surgical operation to removal all or part of the uterus. There are different types of hysterectomy procedures, including:
Vaginal Hysterectomy
This procedure is most often used in cases of uterine prolapse, or when vaginal repairs are necessary for related conditions. During a vaginal hysterectomy, the surgeon detaches the uterus from the ovaries, fallopian tubes, and upper vagina, as well as from the blood vessels and connective tissue that support it. The uterus is then removed through the vaginal opening. If a patient’s uterus is enlarged, a vaginal hysterectomy may not be possible.
Laparoscope-assisted Vaginal Hysterectomy (LAVH)
LAVH uses a laparoscope (a thin, flexible tube containing a video camera) to guide the removal of the uterus and/or fallopian tubes and ovaries through the vagina. During LAVH, several small incisions are made in the abdominal wall through which slender metal tubes known as “trocars” are inserted to provide passage for a laparoscope and other microsurgical tools. Next, the uterus is detached from other structures in the pelvis using the laparoscopic tools. The fallopian tubes and ovaries are also detached from their ligaments and blood supply. The organs and tissue are then removed through an incision made in the vagina. LAVH typically requires a one to three day hospital stay. Complete recovery time is usually four weeks.
Robotic-assisted Laparoscopic Hysterectomy
During a robotic-assisted laparoscopic hysterectomy, a surgeon controls the movements of robotic arms from a computer station in the operating room. Three or four small incisions are made near the belly button. Gas may be pumped into the belly to distend it and give the surgeon a better view and more room to work. The laparoscope is inserted the abdomen, while other surgical instruments are inserted through the other incisions. The uterus will be cut into small pieces that can be removed through the small incisions. Depending on the reasons for a patient’s hysterectomy, the entire uterus may be removed or just the part above the cervix. The fallopian tubes and ovaries attached to the uterus may also be removed. Most people stay in the hospital for a few days. Complete recovery may take anywhere from a few weeks to a few months.
Abdominal Hysterectomy
The uterus is removed through the abdomen via a surgical incision about six to eight inches long. The incision can be made either vertically, from the navel down to the pubic bone, or horizontally, along the top of the pubic hairline. The tissues connecting the uterus to blood vessels and other structures in the pelvis are then carefully cut away. The uterus is removed, along with any other structures such as the ovaries, fallopian tubes, and cervix, depending on each patient’s situation. Abdominal hysterectomy usually requires a hospital stay of one to two days, but it could be longer. The recovery period is usually about six to eight weeks.
Pelvic Congestion Syndrome (PCS)
What is pelvic congestion syndrome?
Pelvic congestion syndrome (PCS) is a condition that causes chronic pelvic pain. This syndrome is thought to be caused by hormonal and physical changes during pregnancy which can lead to buildup of pressure in the veins around ovaries. It occurs most frequently in women between the ages of 20 and 45, more commonly in women with a history of multiple pregnancies. Women are more likely to develop PCS if members of their family have had it.
Symptoms of Pelvic Congestion Syndrome
Common symptoms associated with pelvic congestion syndrome:
- Dull ache or pain in the pelvis or lower back
- Worsening symptoms with standing or during menstruation
- Irritable bladder that makes it hard to control urination
- Discomfort during or after sexual intercourse
- Bulging veins in the inner thighs, butt, vagina and/or vulva
Ovarian Vein Embolization
If you and your healthcare provider determine that you have Pelvic Congestion Syndrome (PCS), it is a good idea to discuss the various treatment options available, including ovarian vein embolization (OVE).
In ovarian vein embolization, an Interventional Radiologist (IR) passes a catheter (small tube) through a vein in the groin using specialized x-ray equipment. Once the catheter is appropriately positioned in the ovarian vein, the vein is blocked using small metallic coils and/or a sclerosing agent (Sotradecol) to seal the vein. This prevents reflux of blood into the pelvis greatly reducing pelvic pain and varices. Once embolization is complete the catheter is removed. The entire treatment typically lasts 1-2 hours and is an outpatient procedure. Recovery typically takes less than one week. Reported success rates are >85%.

Is Ovarian vein embolization right for me?
You may be a candidate if:
- You are experiencing pelvic pain and diagnosed with enlarged ovarian veins
- You do not want to take medications which may impact your hormone levels
- You are experiencing side-effects of medications
- You do not want surgery
- You do not want the potential risks of surgery
- You are a poor surgical candidate
Key Advantages
Ovarian vein embolization is a safe treatment option and like other minimally invasive procedures has significant advantages over conventional open surgery.
Benefits
- Multiple research studies demonstrating significantly improved pelvic pain after embolization
- Same day procedure
- No general anesthesia required
- No risk of hormone changes
- No surgical risk
Potential Risks
- Allergic reaction
- Infection
- Bruising or bleeding at the puncture site
Other Treatment Options
Non-invasive treatment options
- Hormonal medication to block ovarian function and/or pain
Surgical treatment options
- Surgery to block or remove damaged veins
- Hysterectomy to remove the uterus and ovaries